6 popular peanut butters linked to colon cancerStory by Son of Grey Peanut butter is a staple in many households, loved for its creamy texture, nutty flavor, and protein content. However, not all peanut butter is created equal. Certain types of commercially processed peanut butter may contain added sugars, unhealthy oils, and chemical contaminants that studies suggest could increase the risk of colorectal cancer. Understanding which kinds to avoid can help you enjoy peanut butter safely while maintaining a healthy diet. Here’s a look at kinds of peanut butter linked to colon cancer risks. Peanut Butter with Added Hydrogenated OilsMany mass-market peanut butters contain hydrogenated oils to improve shelf life and prevent separation. These trans fats are widely linked to inflammation and increased cancer risk, including colon cancer. Common brands with older formulations that included hydrogenated oils include Skippy Creamy Peanut Butter and Jif Creamy Peanut Butter. While these brands have reformulated many of their products to remove partially hydrogenated oils, older stock and certain varieties may still pose risks. Peanut Butter High in Added SugarsExcessive sugar consumption has been associated with chronic inflammation and insulin resistance, factors that can contribute to colon cancer development. Many flavored or “sweetened” peanut butters—such as Reese’s Peanut Butter Spread or honey-flavored supermarket brands—contain high amounts of added sugar beyond what’s naturally in peanuts. These products are convenient for desserts and snacks but may carry hidden health risks when consumed frequently. Peanut Butter Contaminated with AflatoxinsAflatoxins are naturally occurring toxins produced by molds on peanuts, particularly if storage conditions are poor. Long-term exposure to aflatoxins has been linked to liver cancer and may contribute indirectly to colorectal cancer risk due to systemic inflammation and DNA damage. While major brands like Smucker’s Natural Peanut Butter and Planters Peanut Butter test rigorously for aflatoxins, lower-cost store brands or imported peanut butters may be more likely to contain small amounts of these toxins. Ultra-Processed Peanut ButtersUltra-processed peanut butters often contain a mix of additives, stabilizers, and preservatives that can affect gut health. Poor gut microbiome balance is increasingly recognized as a factor in colon cancer risk. Brands like Peter Pan Extra Crunchy or value-line supermarket peanut butters may include emulsifiers and stabilizers that are generally safe in small amounts but could have cumulative effects over time when consumed daily. Tips for Choosing Safer Peanut ButterOpt for natural or “just peanuts” varieties with no added hydrogenated oils or sugars. Check for aflatoxin testing or certifications from major brands. Store peanut butter properly in a cool, dry pantry or refrigerate to reduce mold growth. Moderate consumption to avoid excess calories, sugars, or unhealthy fats. While peanut butter can be a healthy protein and fiber source, products with hydrogenated oils, added sugars, aflatoxin contamination, or excessive processing may contribute to colon cancer risk. Choosing natural, minimally processed peanut butter from trusted brands like Smucker’s Natural, MaraNatha, or 365 by Whole Foods, and storing it carefully, can help you enjoy this classic snack safely and responsibly. ARTICLE SOURCE: https://www.msn.com/en-us/health/other/6-popular-peanut-butters-linked-to-colon-cancer/ar-AA1WvYFn?




Why Obesity Is Linked to Higher Cancer Rates in Young People
The rates of certain cancers are climbing in young U.S. adults, and it’s not entirely clear why. To make sense of the trend, many scientists are drawing connections to the simultaneous rise of another major public health crisis: obesity.
Younger generations are more likely to develop obesity than ever before. In 2009, about 33% of adults ages 20 to 44 had obesity. By 2020, that number shot up to 41%.1
Having overweight or obesity—a body mass index (BMI) greater than 25—is linked with a higher risk of 13 types of cancer, which account for 40% of cancers diagnosed in the U.S. each year, according to the CDC.2
Scientists have long known that obesity raises the risk of developing and dying of cancer in older adults. More recent research suggests that obesity may also shift the timing of cancer appearance, making it more likely to appear in younger groups.3
“It appears that cancer incidence is rising for young adults and it’s primarily driven by diagnoses of obesity-related cancers. That suggests obesity has something to do with the rise in early onset cancers,” said Karen Basen-Engquist, PhD, MPH, a professor of health disparities and director of the Center for Energy Balance in Cancer Prevention and Survivorship at the MD Anderson Cancer Center.
Between 1995 and 2014, there was an increase in early-onset diagnoses for six of 12 obesity-related cancers, according to a 2019 study. Of the 18 cancers not linked to obesity, only two became more common in young adults.4
The connection between obesity and early-onset cancer crises is multi-faceted. The biological mechanisms are complex—fat tissue itself can encourage cancer to develop and grow by spurring inflammation and cancer-promoting hormones.
Obesity is also related to several chronic conditions, like type 2 diabetes and heart disease, which can exacerbate cancer risk. People with obesity can face social barriers to screening, too, which sometimes lead to more aggressive disease and poorer outcomes.
The 13 types of cancers that are linked to obesity: adenocarcinoma of the esophagus, breast cancer in post-menopausal women, colorectal cancer, uterine cancer, gallbladder cancer, upper stomach cancer, kidney cancer, liver cancer, ovarian cancer, pancreatic cancer, thyroid cancer, meningioma, and multiple myeloma.
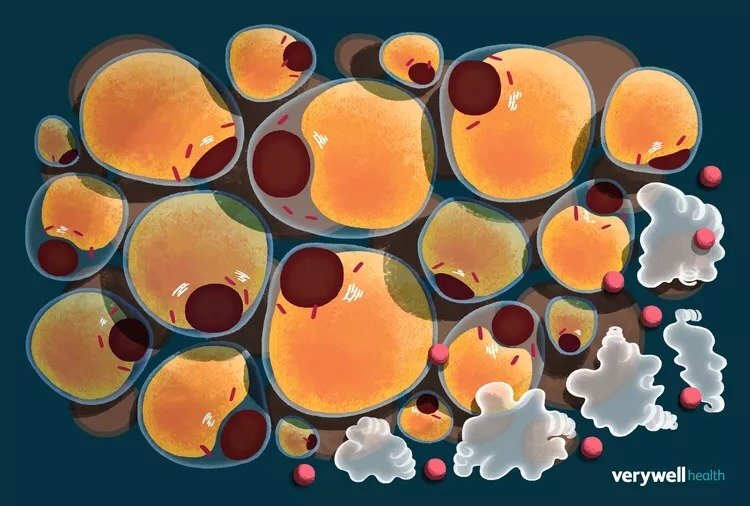
How Does Excess Fat Tissue Contribute to Cancer Growth?
Fat tissue isn’t a single idle organ that only stores energy. Rather, there are several types of fat, each of which produce substances that act like hormones, helping to control metabolism by ushering messages between the fat, brain, immune system, and other organs.
Obesity is commonly defined as the accumulation of too much fat. With excess fat tissue comes an excess of a particular group of proteins called adipokines.5
Adipokines incite inflammation in the fat tissue and sometimes throughout the body. That inflammation can cause cells to mutate and grow quickly, sometimes causing cancer to develop or grow faster.6
Obesity-induced inflammation also leads the body to produce too much insulin. Apart from contributing to obesity, too-high levels of insulin can encourage cells to grow faster and prevent them from their normal process of death and regeneration. This provides more opportunity for mutations that could lead to cancer.
Insulin resistance and high blood sugar create “a recipe for cells to grow,” said Stephen Freedland, MD, a professor of urology and the director of the Center for Integrated Research in Cancer and Lifestyle at Cedars-Sinai Medical Center. High insulin is linked to breast, prostate, and colorectal cancers—some of the cancer types that are becoming increasingly common in young adults.
Fat tissue can also produce excess amounts of the hormone estrogen, especially in women. High levels of estrogen are linked to breast, endometrial, and ovarian cancers.7
Not all cancer behaves the same. The way that obesity factors into the growth of certain cancers will depend on the type and location of the malignancy, according to Basen-Engquist.
“Things like inflammation and the environment that the tumor lives in can affect how fast the tumor growth is promoted,” Basen-Engquist said.
How Does Obesity Complicate Cancer Screening?
Obesity can not only make someone biologically vulnerable to cancer, but may also make it harder to find and treat the disease early on.
In one review paper, some physicians reported lacking the education and tools to effectively perform certain cancer screenings. Patients with obesity, meanwhile, said that factors including embarrassment and experience of previous stigma from healthcare providers stopped them from seeking cancer screening.8
“That [stigma] can make people less willing to come in for screening, particularly screenings where they’re going to have to undress or unclothe in some way, which is most cancer screenings,” Basen-Engquist said.
When people with obesity face barriers to effective screening, early-stage cancers can fly under the radar, sometimes leading them to progress to more aggressive malignancies. That can be especially problematic in adults younger than 40, who are generally not yet eligible for routine cancer screenings.
Providers may need to use special techniques during manual cancer exams in people with obesity, like when palpating larger breasts or performing a rectal exam. Obesity can complicate blood tests, too. People with higher weight tend to have a greater volume of blood, which can dilute the levels of proteins that indicate the presence of certain cancer types.
In the case of blood testing for prostate cancer, it may appear as though obesity protects against prostate cancer when, in fact, cases may go undiagnosed in patients with obesity, Freedland explained. Those cases may progress to be especially aggressive.
“As we get more and more obese as a country, we’re probably missing some prostate cancers, but it’s causing more prostate cancer deaths,” Freedland said
However, improvements in imaging and genetic testing are making these tools less prone to complications from obesity, he added.
How Much Does Weight Management Matter in Reducing Cancer Risk?
While obesity is strongly linked to the rising trends of certain cancers in young adults, the condition is unlikely to fully explain the trend, said Hyuna Sung, PhD, senior principal scientist for cancer surveillance research at the American Cancer Society.
“The causes of cancer are always multifactorial. Increasing obesity may explain just a fraction of the increase in early-onset cancers,” Sung said.
Diet and exercise are often wielded as tools for weight management. But lifestyle choices may independently influence their cancer risk. For instance, certain ultra-processed foods are carcinogenic. Spending a lot of time sitting or laying down, even if you’re of average weight, can increase your cancer risk.
Some evidence suggest that regular aerobic movement can help stave off seven types of cancer.9 That’s especially true for breast, colorectal, and endometrial cancer–three types that are becoming more commonly diagnosed in young adults.10
The Road Ahead for Obesity and Cancer Research
To further understand the relationship, researchers are looking into the role of various types of fat, how the gut microbiome factors in, and why some tumors look different in young and old adults with obesity.
Even body mass index—the tool that providers use to diagnose obesity—may be flawed. BMI only accounts for how heavy someone is relative to their height and doesn’t take body composition into account, Basen-Engquist said.
“A lot of athletes—football players and so forth—may have a BMI over 30, but a lot of it is muscle, so they have less fat tissue to drive those obesity-related mechanisms,” she said.
Fat carried in your midsection tends to be “more dangerous” than fat stored elsewhere, because it can increase inflammation around the organs, Basen-Engquist said. While calculating body composition and waist circumference could give researchers a better understanding of how fat tissue relates to cancer than BMI does, using those measurements in research can be logistically complicated.
Studying the way that obesity influences cancer risk in young people is tricky. Most older adults nowadays didn’t have obesity in their youth, so scientists can’t compare their outcomes to today’s young adults who are more frequently overweight, Freedland said.
There are several outstanding questions. Is it better, for instance, to maintain a normal weight for most of your life and then develop obesity later on, or to have a stable but higher weight over a long time? It’s also not yet clear to what degree losing weight in adulthood after a long period of obesity decreases cancer risk, if at all.
With the introduction of new GLP-1 receptor agonist drugs like Wegovy and Zepbound, answers to those questions may come closer within reach. Research on the effects of these obesity medications could help researchers hone in on how weight and weight management relate to cancer.
“I don’t want to say weight loss is not beneficial—I absolutely think it is. We just don’t have the clear evidence. We’re trying to build that story,” Freedland said. “There are a lot of questions to answer.”
What This Means for You
There's strong evidence that eating a balanced diet and getting adequate exercise can be cancer-preventive. Getting enough sleep, avoiding cigarettes and alcohol, and reducing stress can also reduce your cancer risk.
Organizations like the Obesity Action Coalition and the Obesity Medicine Association can help you connect with obesity-aware providers or obesity medicine experts.
Subscribe to Carnivore Talk on YouTube | Be our guest on the channel | Leave me a voicemail, yo!