Today is the first day of January and is also the first day of World Carnivore Month. To that end, let's challenge ourselves to eat a carnivore diet for the entire month of January. The type of carnivore diet and the level of strictness you choose to do is entirely up to you. Examples of carnivore diets include the following...
1) The Lion Diet. A person eating the Lion Diet only consumes the flesh of ruminant animals, water, and salt.
2) The BBBE Diet. BBBE is an acronym for Beef, Butter, Bacon, and Eggs.
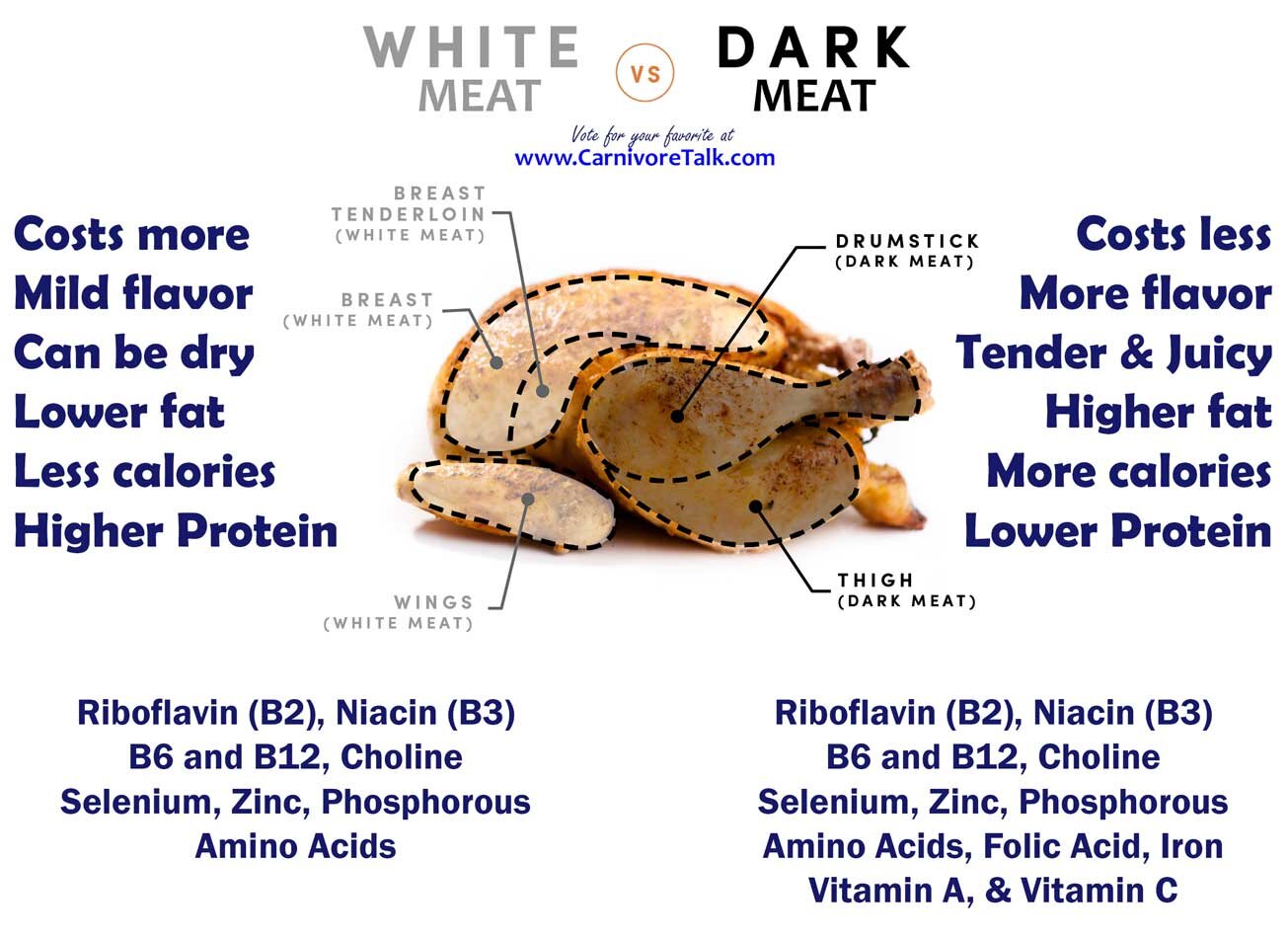
3) The Carnivore Diet. This allows for the consumption of any and all animals and animal by-products, including dairy.
In any of the above examples, the object of course is to not consume any plants as part of your diet. Of course, we're not going to micromanage hoe you prepare your food, so your use of seasonings is entirely your own personal choice.
IF your circumstances don't allow you to go full on carnivore in January, then you can participate in this topic by challenge yourself to do better, above and beyond what you have been doing. For example, if you have still been eating grains, seed oils, refined sugar, or drinking alcohol, challenge yourself to avoid these items and just eat a clean, single ingredient whole foods diet such as clean keto, ketovore, or animal based.
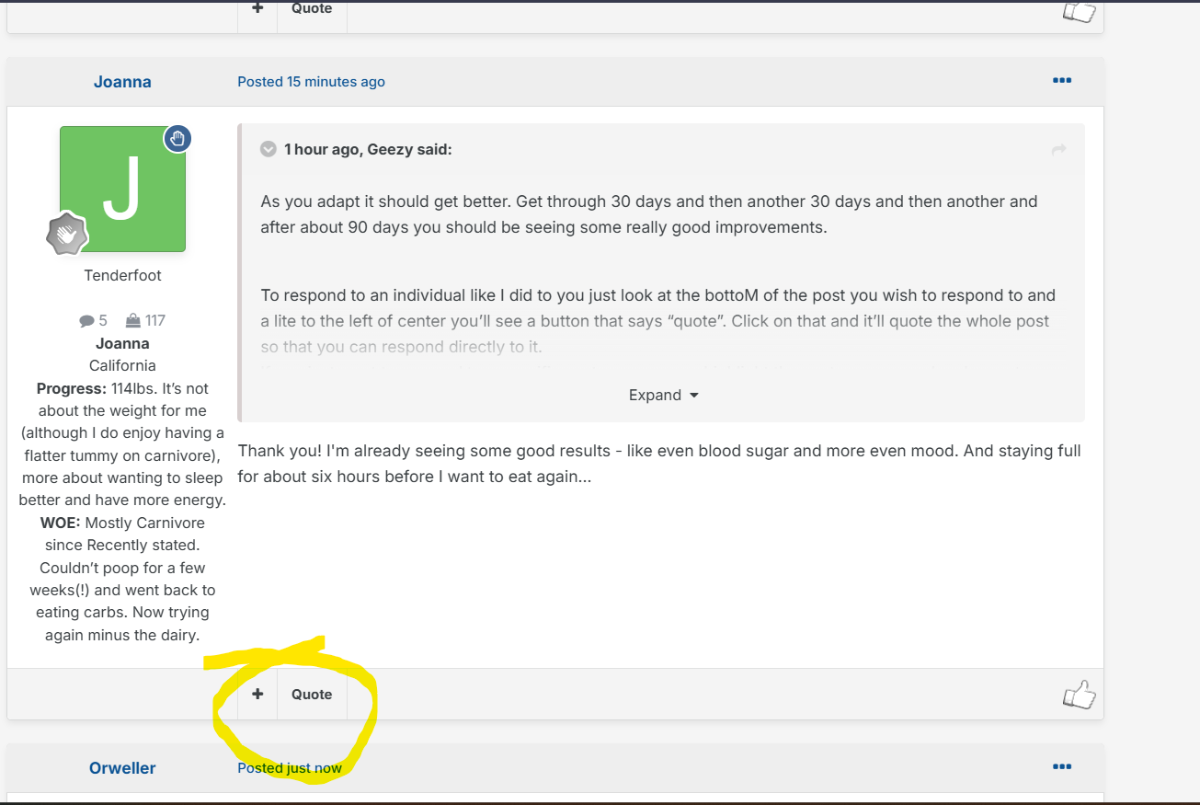
We encourage you to check in daily, and share what you have eaten, perhaps a weigh-in if you're willing, and enjoy in some small talk. Participants in this topic will be entered into a drawing for a prize at the end of the month.





Alzheimer’s may stem from modern lifestyles, new study suggests
Story by BY JUDY SIEGEL-ITZKOVICH
Alzheimer’s disease (AD) – the most common type of dementia – was first discovered by clinical psychiatrist Dr. Alois Alzheimer who described a 50-year-old woman, Auguste Deter, in a Frankfurt psychiatric hospital in 1901.
It affects one person in 14 people over the age of 65. one in every six people over the age of 80, and one in three in people aged 85 and older.
But did AD always affect the population? The Bible – which doesn’t hide illnesses – has no mention of it; some of our forefathers and foremothers (but not Sarah) suffered from vision problems, weakness, and other physical problems at the end of their lives, but nothing about dementia.
Medical texts from 2,500 years ago rarely mention severe memory loss, suggesting today’s widespread dementia stems from modern environments and lifestyles, according to a new study at the University of Southern California.
A mosaic of the Roman goddess of the hunt, Diana, hunting a doe. (credit: Wikimedia Commons)
A new analysis of classical Greek and Roman medical texts suggests that severe memory loss – occurring at epidemic levels today – was extremely rare 2,000 to 2,500 years ago, in the time of Aristotle, Galen, and Pliny the Elder.
The research, published in the Journal of Alzheimer's Disease under the title “Dementia in the Ancient Greco-Roman World Was Minimally Mentioned,” bolsters the idea that Alzheimer’s disease and related dementias are diseases of modern environments and lifestyles, with sedentary behavior and exposure to air pollution largely to blame.
“The ancient Greeks had very, very few – but we found them – mentions of something that would be like mild cognitive impairment,” said first author and gerontologist Prof. Caleb Finch. “When we got to the Romans, and we uncovered at least four statements that suggest rare cases of advanced dementia; we can’t tell if it’s Alzheimer’s. So, there was a progression going from the ancient Greeks to the Romans.”
Historical mentions of memory loss
Ancient Greeks recognized that aging commonly brought memory issues we would recognize as mild cognitive impairment) but nothing approaching a major loss of memory, speech, and reasoning as caused by Alzheimer’s and other types of dementia, he continued.
Finch and co-author Stanley Burstein, a historian at California State University in Los Angeles, pored over a major body of ancient medical writing by Hippocrates and his followers. The text catalogs ailments of the elderly, such as deafness, dizziness, and digestive disorders, but makes no mention of memory loss.
Centuries later, in ancient Rome, a few mentions crop up. Galen remarks that at the age of 80, some elderly begin to have difficulty learning new things. Pliny the Elder notes that the senator and famous orator Valerius Messalla Corvinus forgot his own name. Cicero prudently observed that “elderly silliness … is characteristic of irresponsible old men, but not of all old men.”
The Greeks and Romans were mainly concerned with the physical frailties of older ages. Finch speculates that as Roman cities grew denser, pollution increased, driving up cases of cognitive decline. In addition, Roman aristocrats used lead cooking vessels, lead water pipes and even added lead acetate into their wine to sweeten it – unwittingly poisoning themselves with the powerful neurotoxin.
A few ancient writers recognized the toxicity of lead-containing material, but little progress was made in dealing with the problem until well into the 20th century. Some scholars blame lead poisoning for the fall of the Roman Empire.
For this paper, Finch didn’t just think about the Roman Empire or the Greeks. In the absence of demographic data from these ancient cultures, Finch turned to a surprising model for ancient aging – today’s Tsimane Amerindians, an indigenous people of the Bolivian Amazon.
The Tsimane – like the ancient Greeks and Romans – have a preindustrial lifestyle that is very physically active, and they have extremely low rates of dementia. An international team of cognitive researchers led by psychology and gerontology Prof. Margaret Gatz found among older Tsimane people.
“The Tsimane data, which is serious, is very valuable,” Finch said. “This is the best-documented large population of older people that have minimal dementia, all of which indicates that the environment is a huge determinant on dementia risk. They give us a template for asking these questions.”
ARTICLE SOURCE: https://www.msn.com/en-us/health/medical/alzheimer-s-may-stem-from-modern-lifestyles-new-study-suggests/ar-BB1hK7Dg
Subscribe to Carnivore Talk on YouTube | Be our guest on the channel | Leave me a voicemail, yo!