Today is the first day of January and is also the first day of World Carnivore Month. To that end, let's challenge ourselves to eat a carnivore diet for the entire month of January. The type of carnivore diet and the level of strictness you choose to do is entirely up to you. Examples of carnivore diets include the following...
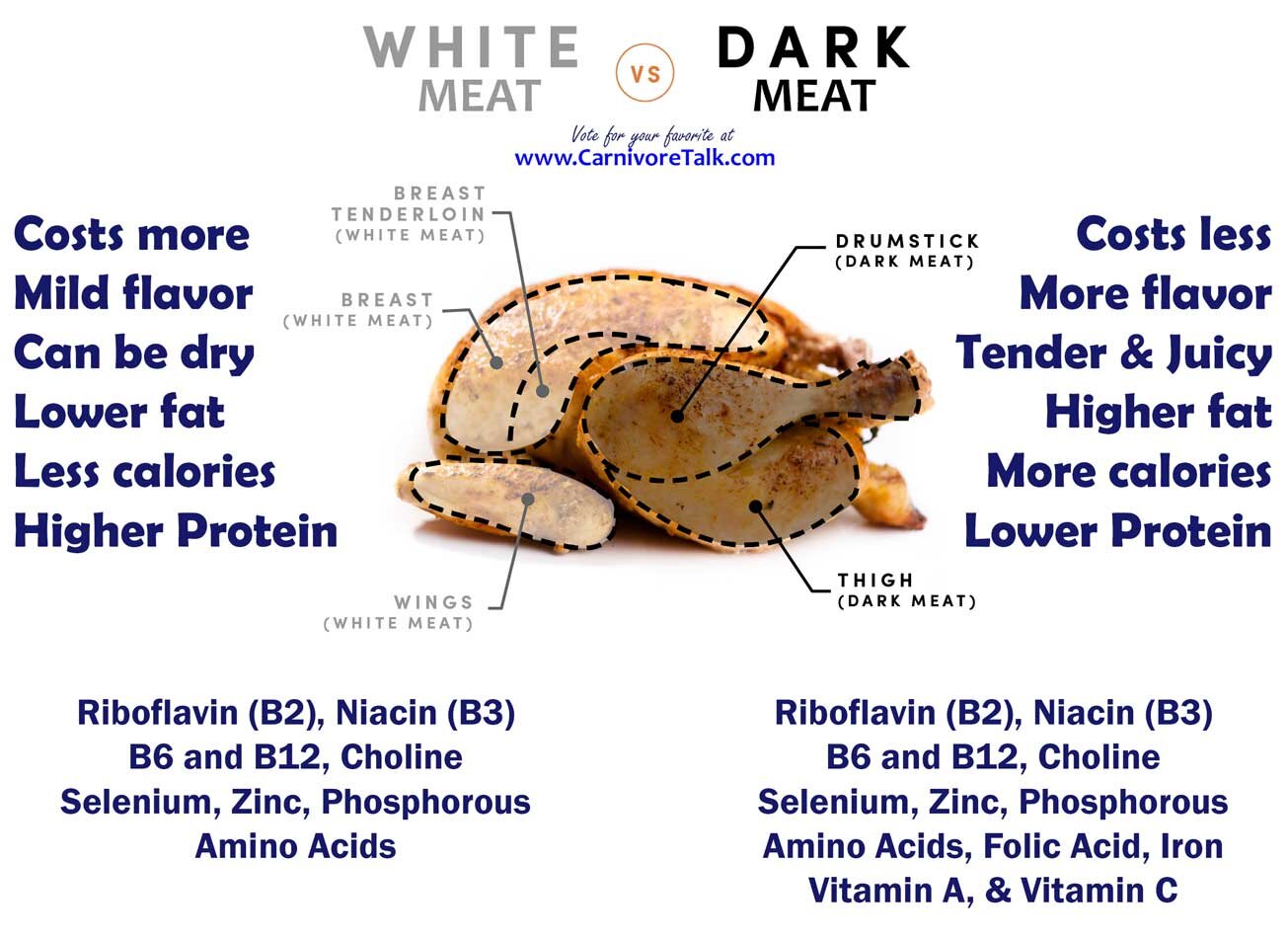
1) The Lion Diet. A person eating the Lion Diet only consumes the flesh of ruminant animals, water, and salt.
2) The BBBE Diet. BBBE is an acronym for Beef, Butter, Bacon, and Eggs.
3) The Carnivore Diet. This allows for the consumption of any and all animals and animal by-products, including dairy.
In any of the above examples, the object of course is to not consume any plants as part of your diet. Of course, we're not going to micromanage hoe you prepare your food, so your use of seasonings is entirely your own personal choice.
IF your circumstances don't allow you to go full on carnivore in January, then you can participate in this topic by challenge yourself to do better, above and beyond what you have been doing. For example, if you have still been eating grains, seed oils, refined sugar, or drinking alcohol, challenge yourself to avoid these items and just eat a clean, single ingredient whole foods diet such as clean keto, ketovore, or animal based.
We encourage you to check in daily, and share what you have eaten, perhaps a weigh-in if you're willing, and enjoy in some small talk. Participants in this topic will be entered into a drawing for a prize at the end of the month.




Red meat may not cause harmful inflammation after all
OCTOBER 27, 2023
by John Anderer
HOUSTON — A little inflammation is usually a positive sign the immune system is at work, but chronic inflammation can take a heavy toll on the body’s cells, tissues, and organs. Doctors have long advised patients to avoid eating too much red meat as a means of avoiding chronic inflammation, but have burgers and steaks gotten a bad rap? Researchers from Baylor College of Medicine say red meat may not be so bad after all.
“The role of diet, including red meat, on inflammation and disease risk has not been adequately studied, which can lead to public health recommendations that are not based on strong evidence,” says Dr. Alexis Wood, associate professor of pediatrics – nutrition at the USDA/ARS Children’s Nutrition Research Center at Baylor College of Medicine and Texas Children’s Hospital, in a university release. “Our team sought to take a closer look by using metabolite data in the blood, which can provide a more direct link between diet and health.”
To study this topic, the research team analyzed cross-sectional data encompassing roughly 4,000 older adults participating in the Multi-Ethnic Study of Atherosclerosis (MESA). For reference, cross-sectional data is quite useful as a source of evidence on how diet affects health, as it makes use of data observed with free-living people, without any attempts to influence their usual lifestyle.
In this way, study authors believe it may be easier to take results from such earlier studies and apply them to non-research settings. Meanwhile, besides just assessing participants’ self-reported food intake and several biomarkers, the research team also gauged a large array of dietary intake metabolites in their blood. Plasma metabolites are useful in terms of assessing the effects of dietary intake as food is processed, digested, and ultimately absorbed into the body.
After adjusting for body mass index (BMI), researchers concluded the ingestion of unprocessed and processed red meat (beef, pork, or lamb) was not directly associated with any markers of inflammation. Researchers theorize this suggests body weight, not red meat, may be the real driving force behind increased systemic inflammation. Importantly, no link was seen connecting red meat intake and C-reactive protein (CRP), considered the major inflammatory risk marker of chronic disease.
“Our analysis adds to the growing body of evidence that indicates the importance of measuring plasma markers, such as metabolites, to track diet and disease risk associations, versus relying on self-reported dietary intake alone,” Dr. Wood explains. “Our analysis does not support previous observational research associations linking red meat intake and inflammation.”
Since observational studies, by their very nature, cannot establish cause and effect, researchers recommend that randomized controlled trials (RCTs) be conducted in the future to confirm these findings. Such trials should entail participants being randomly assigned to either consume a dietary factor of interest or not eat it. Several earlier RCTs have already demonstrated that lean unprocessed beef can be enjoyed as part of certain heart-healthy dietary patterns.
“We have reached a stage where more studies are needed before we can make recommendations to limit red meat consumption for reducing inflammation if we want to base dietary recommendations on the most up-to-date evidence,” Dr. Wood concludes. “Red meat is popular, accessible and palatable – and its place in our diet has deep cultural roots. Given this, recommendations about reducing consumption should be supported by strong scientific evidence, which doesn’t yet exist.”
[hr]
Article Source: https://studyfinds.org/red-meat-inflammation/
Subscribe to Carnivore Talk on YouTube | Be our guest on the channel | Leave me a voicemail, yo!