Today is the first day of January and is also the first day of World Carnivore Month. To that end, let's challenge ourselves to eat a carnivore diet for the entire month of January. The type of carnivore diet and the level of strictness you choose to do is entirely up to you. Examples of carnivore diets include the following...
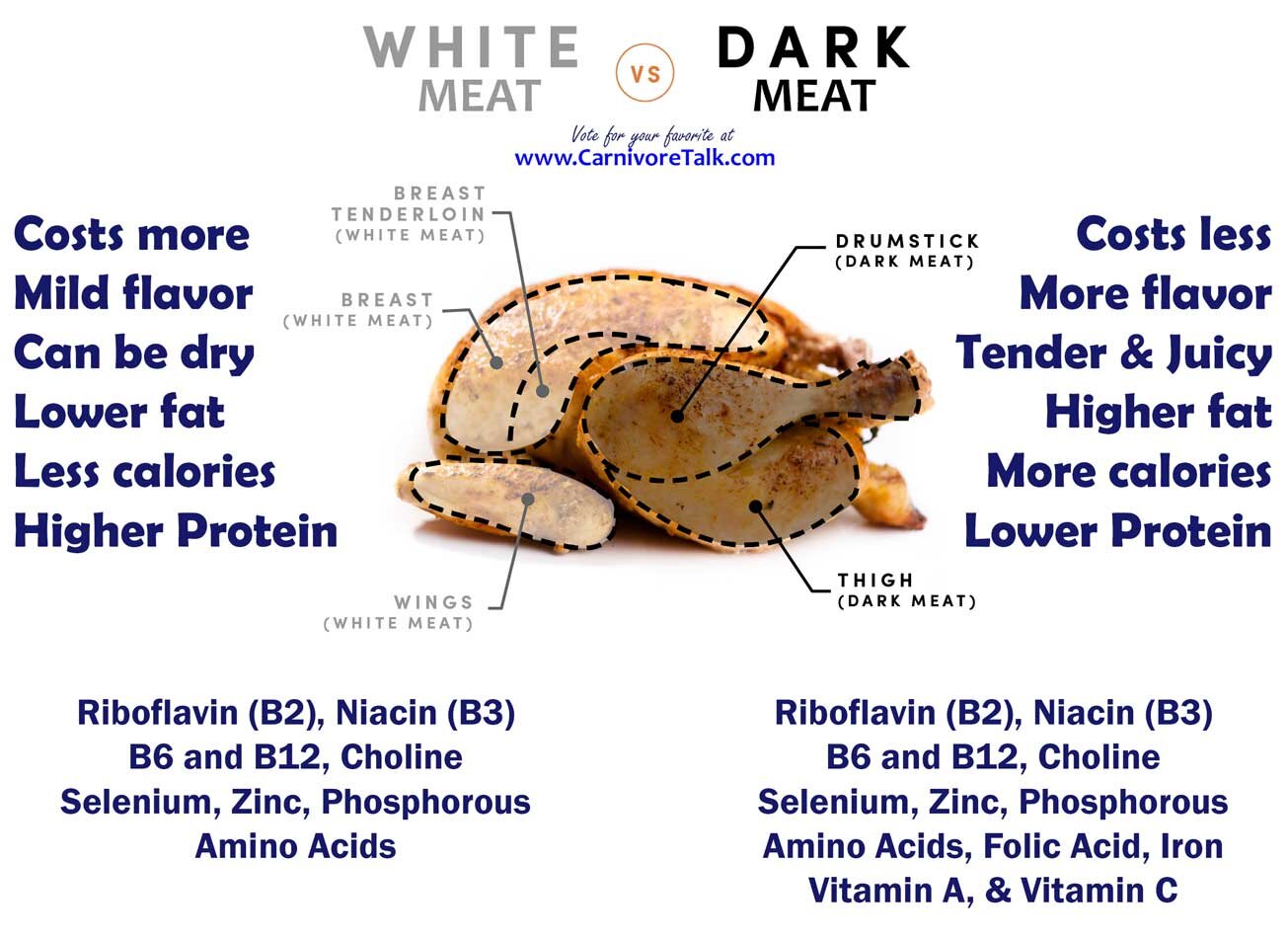
1) The Lion Diet. A person eating the Lion Diet only consumes the flesh of ruminant animals, water, and salt.
2) The BBBE Diet. BBBE is an acronym for Beef, Butter, Bacon, and Eggs.
3) The Carnivore Diet. This allows for the consumption of any and all animals and animal by-products, including dairy.
In any of the above examples, the object of course is to not consume any plants as part of your diet. Of course, we're not going to micromanage hoe you prepare your food, so your use of seasonings is entirely your own personal choice.
IF your circumstances don't allow you to go full on carnivore in January, then you can participate in this topic by challenge yourself to do better, above and beyond what you have been doing. For example, if you have still been eating grains, seed oils, refined sugar, or drinking alcohol, challenge yourself to avoid these items and just eat a clean, single ingredient whole foods diet such as clean keto, ketovore, or animal based.
We encourage you to check in daily, and share what you have eaten, perhaps a weigh-in if you're willing, and enjoy in some small talk. Participants in this topic will be entered into a drawing for a prize at the end of the month.





Insulin resistance from high-sugar diet may lead to brain decline
By Corrie Pelc on November 8, 2023 — Fact checked by Brittney M. Mikell, PharmD, RPh
Neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS), affect millions of people worldwide.
Although scientists are still unclear as to what the main cause is for many neurodegenerative disorders, they do know certain risk factors play a role.
Research has previously shown that one risk factor for developing a neurodegenerative condition is obesity. However, how obesity increases neurodegenerative disease risk has been unclear.
Now researchers from the Fred Hutch Cancer Center are shedding some light on the mechanisms behind obesity and neurodegenerative disease risk. Using a common fruit fly model, the researchers believe a high-sugar diet causes insulin resistance in the brain, reducing the brain’s ability to remove neuronal debris, thus increasing neurodegeneration risk.
This study was recently published in the journal PLOS Biology.
According to Dr. Akhila Rajan, an associate professor in the Basic Sciences Division of the Fred Hutch Cancer Center and senior author of this study, while human clinical studies have found that obesity is an independent risk factor for neurodegenerative disorders, the direct causative mechanisms that connect diet-induced obesity to impaired brain function is largely unknown.
“Consuming processed food doesn’t just affect weight gain, it affects cognitive function,” Dr. Rajan explained to Medical News Today.
“Using the fruit fly model, my lab previously established that prolonged exposure to increased sugars can contribute to insulin resistance in peripheral tissues. Given that we had a good system to study (the) effect of obesogenic diet exposure, we sought to address how it affects brain function,” she noted.
For this study, Dr. Rajan and her team used a model of the common fruit fly because there are similarities between genes in humans and fruit flies.
“Flies serve as an invaluable genetic model for scientific exploration,” Dr. Rajan said. “We aim to harness the power of this model to understand the impact of diet-induced insulin resistance on cognitive function.”
Researchers focused on studying how a high-sugar diet affected the glial cells, a type of brain cell that provides support and protection to neurons.
Additionally, glial cells are responsible for cleaning up dead neurons or “neuronal debris” from the brain.
During the study, researchers found a protein called PI3k, which indicates how much a cell can respond to insulin.
Researchers found that in a high-sugar diet, the glial cells had reduced amounts of PI3k protein, indicating insulin resistance. Scientists also found the glial cells had a lower amount of another protein called Draper, which normally assists with the clearing of neuronal debris.
Ultimately this stopped the glial cells from removing neuronal waste from the brain.
“What we showed is that when flies are fed an obesity-inducing diet — in their case a diet loaded with 30% more sugar for three weeks — the glial cells are unable to clear neuronal debris,” Dr. Rajan said. “Prior to our study, it was unclear if glial cells can develop diet-based insulin resistance. Our study provided missing evidence that glial insulin resistance, that develops in fly central brain cells, has consequences to glia’s debris-clearing role.”
“Our studies are done using fruit flies,” she continued. “While we can provide new insights into what is likely to happen at a cell biological level, many more years of work needs to be done before we can be sure that similar issues apply in humans. Having said that, at least the surface level implications of our work suggest that maintaining insulin sensitivity in patients prone to dementia, even if they are not diabetic, may be beneficial to promote their nervous system function.”
After reviewing this study, Dr. Raphael Wald, a neuropsychologist with Marcus Neuroscience Institute, part of Baptist Health South Florida, at Boca Raton Regional Hospital, told MNT that this research provides another pathway in which obesity can be a risk factor for neurodegenerative disorders.
“The message is clear that obesity is dangerous in many different ways,” Dr. Wald continued. “This study provides further incentive for doctors and patients to focus on a healthy diet and exercise for patients. Patients may be more willing to make lifestyle changes with this knowledge in hand.”
MNT also spoke with Dr. Manisha Parulekar, director of the Division of Geriatrics at HackensackUMC, co-director of the Center for Memory Loss and Brain Health, and associate professor at Hackensack Meridian School of Medicine, also not involved in the study:
“We know a lot about type 2 diabetes (and) various lifestyle interventions to help reduce the incidence,” Dr. Parulekar continued. “This adds even more urgency to those interventions. It also highlights the importance of social determinants of health even further from population health perspectives. If we want people to utilize these lifestyle changes, we have to make sure that everyone has equal access to these interventions.”
When asked about what the next steps in this research will be, Dr. Rajan said while the current study is focused on cell biological outcomes in glia, their future work will be oriented toward understanding the behavioral outcomes as well.
“For instance, it is possible to run memory tests in flies and other behaviors as well,” she continued. “Ultimately, our goal is to unravel the intricate interplay between diet and the brain.”
Dr. Wald said he would like to see this process demonstrated in humans so that we confirm what we now strongly suspect to be the case.
“Once this is accomplished we can start to work toward new therapies aimed at reducing these risks,” he added.
And Dr. Parulekar commented that there are multiple lifestyle modification studies both completed and in process. However, the starting age for most of these studies is around age 50.
“Do we need to start these interventions even early?” she said. “We would want to learn from some of the newer diabetic medications, are they beneficial if started early on.”
ARTICLE SOURCE:
https://www.medicalnewstoday.com/articles/insulin-resistance-high-sugar-diet-links-obesity-with-dementia
Subscribe to Carnivore Talk on YouTube | Be our guest on the channel | Leave me a voicemail, yo!